
 Revenue Cycle Management
Revenue Cycle ManagementDiscover RCM Best Practices 2026 for Steady Cash Flow

Content
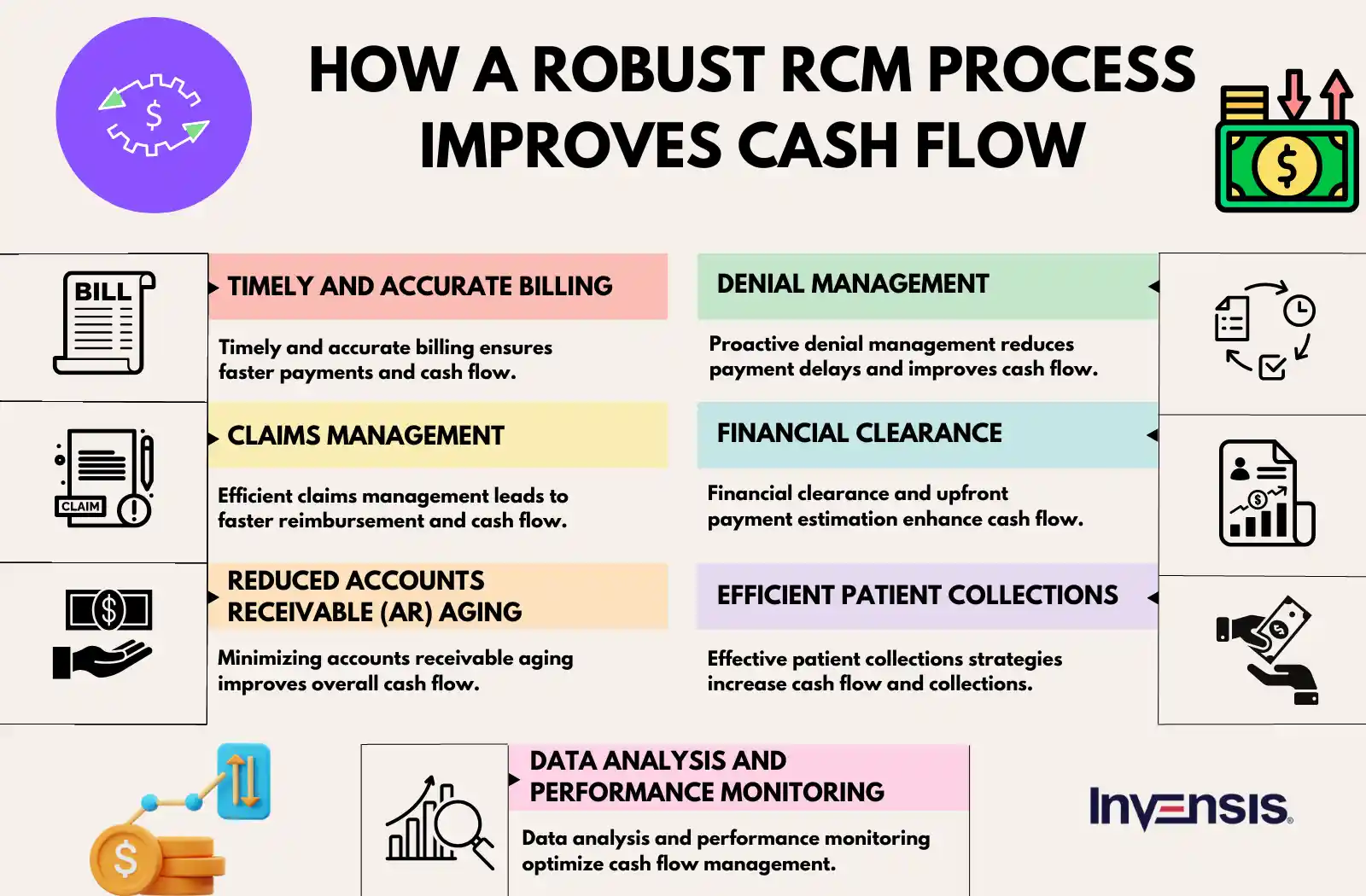
Cash flow and medical Revenue Cycle Management (RCM) are closely interconnected in healthcare. Effective RCM practices directly impact the cash flow of healthcare organizations. Streamlining the revenue cycle, from patient registration to claims submission and reimbursement, reduces claim rejections, denials, and payment delays. This results in faster revenue collection and improved cash flow.
A good example to substantiate this interconnection is the way cash flow got affected across hospitals during the COVID-19 pandemic. The suddenness of the outbreak, the deluge of patients, and the shortage of staff led to inaccurate documentation by and large, inordinate delay in claims submission, gaps in eligibility verification, and a stupendous rise of claims denials had a crippling effect on cash flows. Hospitals were struggling to maintain equipment, get medical supplies on time and pay for staff.
Ensuring steady cash flow boils down to one thing: efficient management of the RCM process. Efficient management can assist organizations in minimizing errors, accelerating reimbursement, and improving overall cash flow. This blog discusses several RCM practices that assist in improving the overall cash flow of the healthcare business.
The Pressing Need for Cash Flow Optimization in Healthcare
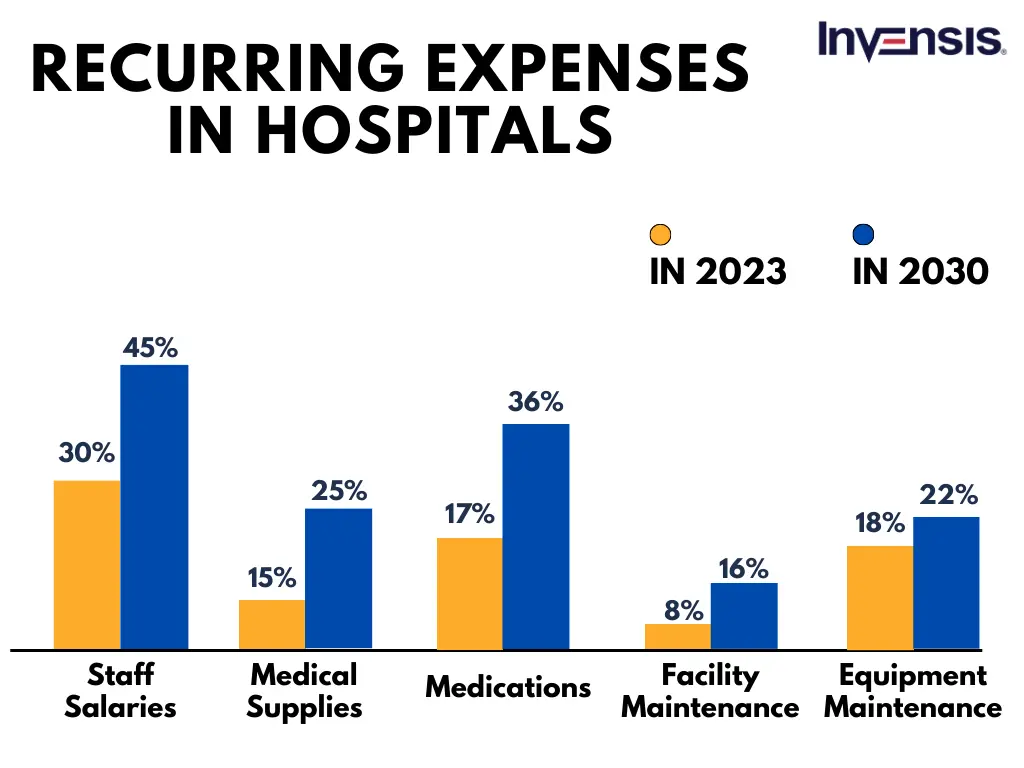
Cash flow optimization is crucial for business sustenance. Healthcare providers need to balance the inflow and outflow of funds while ensuring the delivery of quality patient care and maintaining financial stability. By maintaining a positive cash flow, healthcare businesses can ensure consistent revenue inflow, allowing organizations to provide necessary resources for patient care.
It enables timely payments to suppliers, staff, and vendors, maintaining essential relationships. Adequate cash flow also supports investments in equipment and staff training, enhancing the delivery of high-quality healthcare. Conversely, poor cash flow can lead to delayed payments, limited resources, and compromised patient care. Therefore, managing and improving cash flow is essential for sustaining financial stability and delivering optimal care in healthcare organizations.
Additionally, healthcare organizations need to manage the fluctuations in patient volume and revenue. Seasonal variations, unexpected emergencies, or changes in patient demographics can impact the flow of patients and revenue, leading to cash flow uncertainties. By optimizing cash flow, healthcare businesses can better anticipate and manage these fluctuations, ensuring they have sufficient funds to cover expenses during low-volume periods.

Why Should Best Practices be Followed in RCM?
Following RCM best practices is crucial for several reasons. First, it ensures efficiency and accuracy in the billing and collection processes, leading to timely and maximized revenue capture. Second, adherence to RCM best practices helps minimize claim denials and rejections, reduce revenue leakage, and improve cash flow.
Third, it promotes compliance with regulatory requirements and industry standards, mitigating legal and financial risks. Fourth, RCM best practices support data integrity and reporting accuracy, enabling informed decision-making and strategic planning. Finally, consistently implementing best practices fosters a culture of continuous improvement, driving operational excellence and enhancing overall financial performance in healthcare organizations.
Key RCM Best Practices for Improved Cash Flow in 2026
Effective revenue cycle management (RCM) is crucial for the financial success of healthcare organizations. By implementing the below practices, healthcare businesses can optimize their revenue cycle processes and enhance financial performance.
1. Patient Registration
Patient registration is the crucial first step in the RCM process. Errors in information, such as wrong social ID, can lead to billing issues, payment delays, or denials. To ensure smooth cash flow, follow best practices.
- Ensure staff members emphasize the importance of capturing complete and up-to-date patient information during the registration process.
- Develop strategies to verify insurance coverage and eligibility upfront, such as using online eligibility verification tools or contacting insurance agencies directly.
- Implement training programs to educate staff on the significance of accurate data entry and the potential impact on cash flow.
2. Coding and Documentation
Coding and documentation are pivotal in ensuring proper reimbursement and cash flow. Inaccurate or erroneous coding leads to denial or delays in payment. The following practices will help you maintain effective coding and documentation.
- Train coding and clinical staff on the latest coding guidelines and documentation requirements to ensure compliance.
- Conduct regular audits to identify coding errors or documentation gaps and provide targeted feedback and training to address them.
- Implement technology solutions, such as computer-assisted coding (CAC) systems, to improve accuracy and efficiency.

3. Claims Submission
Timely and accurate submission of claims increases the chances of complete reimbursements and reduced denials. Delayed submissions will lead to delays or claims rejections. By following the below practices, healthcare businesses can submit their claims on time and accurately.
- Establish internal processes for conducting claim reviews before submission to identify and resolve potential issues.
- Monitor and track claim submission metrics to identify patterns or trends that may lead to denials and take proactive steps to address them.
- Leverage technology tools, such as claim scrubbing software, to automatically validate claims for errors or missing information.
According to Change Healthcare, out of $3 trillion in medical claims submitted by US hospitals in 2016, an estimated 9% of charges, representing $262 billion, were initially denied
4. Payment Processing
To maintain a positive cash flow, payment processing should be monitored. Inaccuracies, discrepancies in the payment posting, and irregular follow-up will lead to payment delays. To avoid such issues, follow the below practices and improve cash flow.
- Implement electronic remittance advice (ERA) to receive detailed payment information electronically, streamlining the reconciliation process.
- Automate payment posting and reconciliation processes using technology solutions to minimize manual errors and improve efficiency.
- Encourage patients to opt for electronic funds transfer (EFT) for faster and more secure payment processing.

5. Denial Management
Without identifying the reasons for the denial, resubmission will be ineffective. To tackle and manage the issues, effectively managing the denied claims is important. The following set of practices helps you effectively manage denials and streamline the process to resolve or avoid denials.
- Conduct root cause analysis to identify common denial reasons and address the underlying issues.
- Implement denial prevention strategies, such as improving coding and documentation practices, conducting regular training, and staying updated on payer policies and guidelines.
- Establish strong communication channels with payers to resolve denials promptly and efficiently, including timely filing appeals and providing necessary supporting documentation.
6. Performance Monitoring and Analytics
For optimizing the cash flow, the RCM cycle performance should be monitored. Managing your revenue without achieving the KPIs and making the right decisions will be difficult. Here are some best practices to be followed for revenue growth.
- Implement RCM dashboards and reporting tools to monitor KPIs related to claim submission, payment processing, denials, and reimbursement rates.
- Regularly review and analyze data to identify bottlenecks, inefficiencies, or areas where revenue leakage may occur.
- Use insights from analytics to make informed decisions, implement process improvements, and optimize the revenue cycle management workflow.

Conclusion
While RCM best practices can help you get on top of your cash flow requirements, sustaining effective RCM can be challenging due to the ever-evolving healthcare landscape with changing regulations, coding requirements, and reimbursement policies. Staying compliant necessitates ongoing training, resource allocation, and process adjustments.
RCM involves multiple stakeholders, such as providers, insurers, and patients, requiring coordination amidst diverse systems and communication channels. Technological advancements and system integration complexities demand substantial investment and expertise. Overcoming these challenges is possible only when you have the support of a strategic partner for your needs.
Invensis has vast experience assisting healthcare providers in improving cash flow and financial management through sustained revenue cycle management services. We stay updated with changing regulations, invest in ongoing training, and allocate necessary resources to keep your finances in the pink of health.
Contact us today to discuss how we can improve your RCM operations!
Discover Our Full Range of Services
Click HereExplore the Industries We Serve
Click HereBlog Category
Related Articles

Optimize your store in 2026 with the best WooCommerce order management plugins. Automate order tracking, inventory, and customer service for success.
January 21, 2026
|

Find the leading accounting firms in Singapore trusted by businesses for audit, tax, and advisory services.
November 6, 2025
|

Explore the leading accounting firms in South Africa providing expert audit, tax, cloud accounting, and payroll services. Learn about their key features and unique offerings.
February 2, 2026
|
Services We Provide
Industries We Serve





.webp)