
 Revenue Cycle Management
Revenue Cycle ManagementClaims Scrubbing in Medical Billing - Significance and Ways to Improve

Content
Claims scrubbing in medical billing is the process of electronically reviewing and validating healthcare claims before they are submitted to insurance payers for reimbursement. It involves running the claims through automated software or systems that identify and flag errors, inconsistencies, or missing information that could potentially lead to claim denials or delays in payment. Any discrepancies found during scrubbing are flagged for correction, enabling providers to address issues proactively and resubmit clean claims. Implementing claim scrubbing as a part of the medical billing process is a proactive approach to RCM.
In this blog, we will delve into the importance of claims scrubbing in medical billing and ways to implement it in medical claims processing effectively.
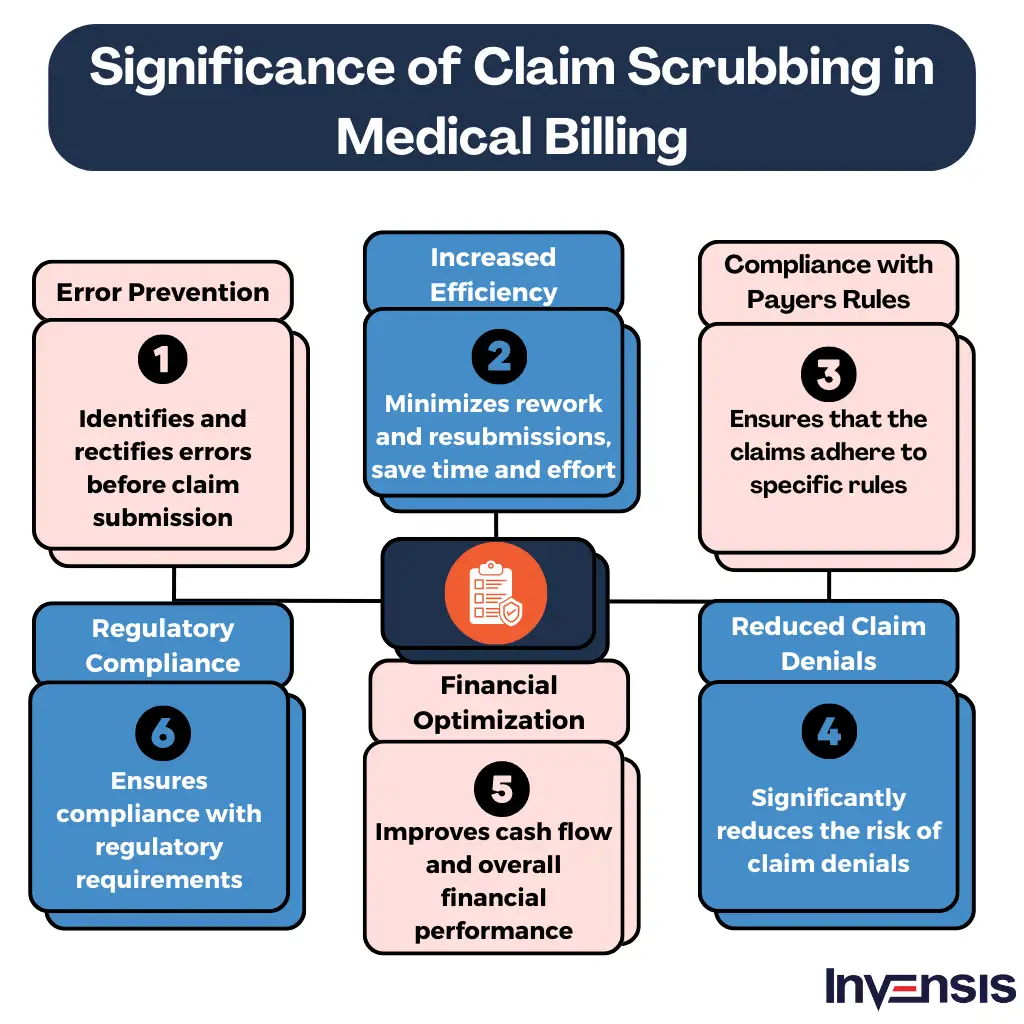
The Significance of Claims Scrubbing in Medical Billing
Claims scrubbing is important because it offers the following benefits:
1. Error Prevention
Claims scrubbing in medical billing helps identify and rectify errors, such as missing or incorrect patient information, incorrect coding, or incomplete documentation, before claims are submitted. By catching these errors early on, providers can reduce the chances of claim denials and delays, ultimately increasing revenue cycle productivity through effective medical billing services.
2. Increased Efficiency
Scrubbing claims before submission ensures that they meet the specific requirements of different payers. This helps minimize rework and resubmissions and saves time and effort for both the healthcare provider and the insurance payer. It also streamlines the billing process and accelerates reimbursement timelines.
3. Compliance with Payer Rules
Different insurance payers have specific rules and guidelines that must be followed when submitting claims. Claims scrubbing in medical billing ensures that the claims adhere to these rules, preventing potential non-compliance issues. This includes checking for correct coding, modifier usage, and medical necessity documentation.
4. Reduced Claim Denials
By identifying and addressing errors or inconsistencies, claims scrubbing significantly reduces the risk of claim denials. It helps ensure that claims are accurate, complete, and meet the specific requirements of insurance payers. This leads to a higher rate of clean claims, increasing the likelihood of timely and accurate reimbursement.
5. Financial Optimization
Effective claims scrubbing in medical billing results in higher first-pass acceptance rates, reducing the need for costly and time-consuming appeals or rework. It maximizes revenue by minimizing denials and payment delays, improving cash flow and overall financial performance for healthcare providers.
6. Regulatory Compliance
Claims scrubbing also plays a key role in ensuring compliance with regulatory requirements, including HIPAA, by verifying that patient information and documentation are appropriately handled and protected.
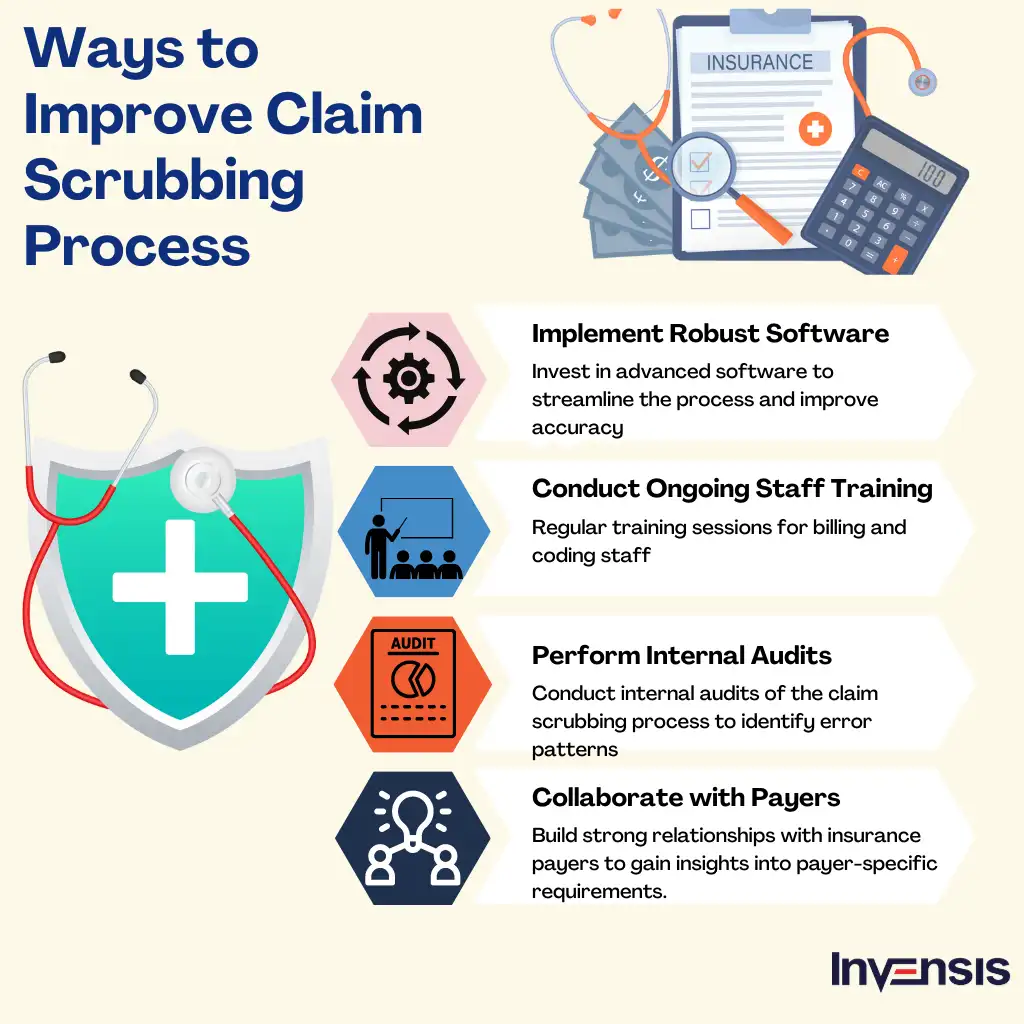
How to Improve Claims Scrubbing Process?
Healthcare providers can enhance the claim scrubbing process in several ways:
1. Implement Robust Software
Investing in advanced claims scrubbing software helps healthcare providers streamline the process and improve accuracy. These tools utilize automated algorithms to detect errors and inconsistencies, ensuring claims are clean before submission.
2. Conduct Ongoing Staff Training
Regular training sessions for billing and coding staff help practices stay updated with the latest coding guidelines and payer requirements. Well-trained staff are more equipped to identify potential errors and resolve issues during the claim scrubbing process.
3. Perform Internal Audits
Conducting internal audits of the claim scrubbing in the medical billing process allows providers to identify patterns of errors, areas of improvement, and training needs. This feedback loop helps refine the process and ensure ongoing accuracy and compliance.
4. Collaborate with Payers
Building strong relationships with insurance payers can help healthcare providers gain insights into payer-specific requirements. Also, regular communication and feedback exchanges can minimize claim rejections and denials.
Conclusion
Claim processing in the healthcare industry is becoming increasingly complex due to various factors. Evolving regulatory requirements, changing payer policies, and advancements in medical technology contribute to the growing complexity. New codes and guidelines, such as ICD-10, require meticulous documentation and coding accuracy.
Even payers implement stricter scrutiny, which leads to increased claim denials and appeals. Additionally, the rise in value-based care models and complex reimbursement structures adds further intricacy to the process. To navigate this complexity, healthcare providers must stay updated, invest in robust technology, and consider delegating the task to experienced professionals who can handle the intricacies of claims processing efficiently.
Invensis has over 24 years of experience in providing claims scrubbing support services to healthcare providers. We provide access to specialized expertise, scalable resources, and improved efficiency. It allows healthcare providers to focus on core patient care while ensuring that their claim scrubbing in the medical billing process is handled by professionals with in-depth knowledge of payer requirements and industry best practices. Get in touch with us now to overcome the difficulties of claim processing and streamline your RCM process.
Frequently Asked Questions
Discover Our Full Range of Services
Click HereExplore the Industries We Serve
Click HereBlog Category
Related Articles

Optimize your store in 2026 with the best WooCommerce order management plugins. Automate order tracking, inventory, and customer service for success.
January 21, 2026
|

Find the leading accounting firms in Singapore trusted by businesses for audit, tax, and advisory services.
November 6, 2025
|

Explore the leading accounting firms in South Africa providing expert audit, tax, cloud accounting, and payroll services. Learn about their key features and unique offerings.
February 2, 2026
|
Services We Provide
Industries We Serve





.webp)