
 Revenue Cycle Management
Revenue Cycle ManagementWhat Does a Medical Biller Do ? How to Make Them More Efficient

Content
A medical biller plays a vital part in the administrative and financial aspects of healthcare facilities. They handle the primary responsibility of translating medical services into billing claims, ensuring accurate and timely reimbursement from insurance companies and patients. They also work closely with medical coders, administrative staff, and insurance companies to maintain the operations and financial health of healthcare providers.
Here in this blog, we will discuss what does a medical biller do and essential strategies to enhance a medical biller’s efficiency.
What is a Medical Biller?
A medical biller is a professional who manages the billing process within the healthcare industry, serving as a vital link between healthcare providers and insurance companies. They ensure that healthcare services are properly coded and submitted for reimbursement, translating medical procedures and diagnoses into standardized billing codes.
Medical billers play a crucial role in ensuring the financial health of healthcare practices by accurately processing claims and handling payment details. Their work supports the smooth operation of medical facilities and helps patients navigate the often complex world of healthcare payments.
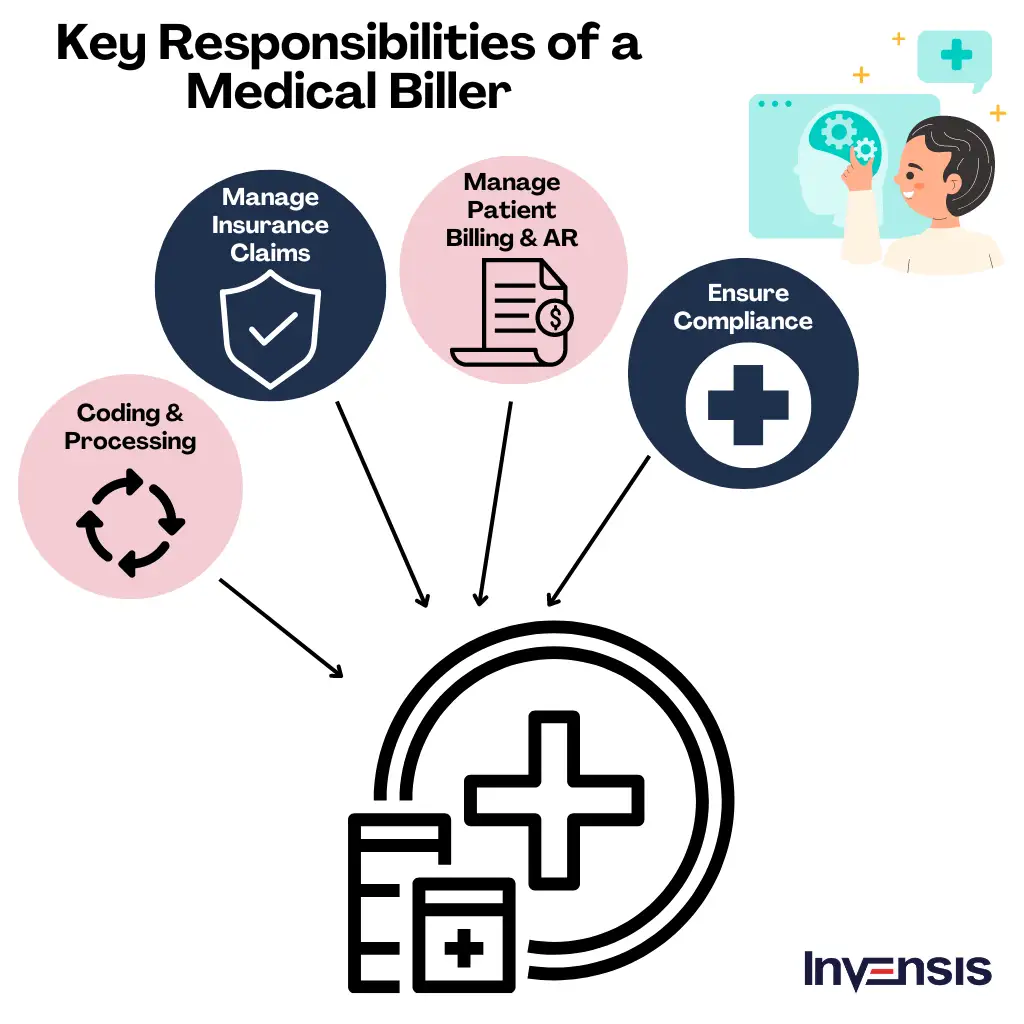
Key Responsibilities of A Medical Biller
The responsibilities of a medical biller encompass a wide range of tasks that contribute to the financial stability of healthcare facilities and practices. Here are the key responsibilities of a medical biller:
1. Code and Process Medical Procedures
One of the key responsibilities of a medical biller is to accurately code and process medical procedures and solutions. They translate complex medical terminology and procedures into universally recognized codes, such as the Current Procedural Terminology (CPT) and the International Classification of Diseases (ICD). Accurate coding ensures that healthcare partners are appropriately reimbursed for the care they provide, minimizing the risk of revenue loss.
2. Handle Insurance Claims
Another vital aspect of a medical biller's role is to handle insurance claims. They gather and organize all necessary patient and insurance information, verify coverage, and submit claims to insurance companies for reimbursement. This process requires a deep understanding of insurance policies, claim submission guidelines, and the ability to navigate complex billing systems. A skilled medical biller ensures that claims are submitted accurately and in a timely manner, maximizing the chances of reimbursement.
3. Manage Patient Billing & Accounts Receivable
Medical billers play a significant role in managing patient billing and accounts receivable. They generate and send invoices to patients, track payments, and address any billing inquiries or disputes. By maintaining open communication with patients, they help clarify billing concerns, explain insurance coverage, and establish payment plans if needed. Effective patient billing ensures the timely collection of payments, contributing to the financial stability of healthcare providers.
4. Ensure Compliance with Healthcare Regulations
Medical billers also ensure compliance with healthcare regulations and standards. They must stay updated with ever-changing healthcare laws, such as the Health Insurance Portability and Accountability Act (HIPAA) and the Affordable Care Act (ACA). By adhering to these regulations, medical billers protect patient privacy and maintain the integrity of healthcare data.
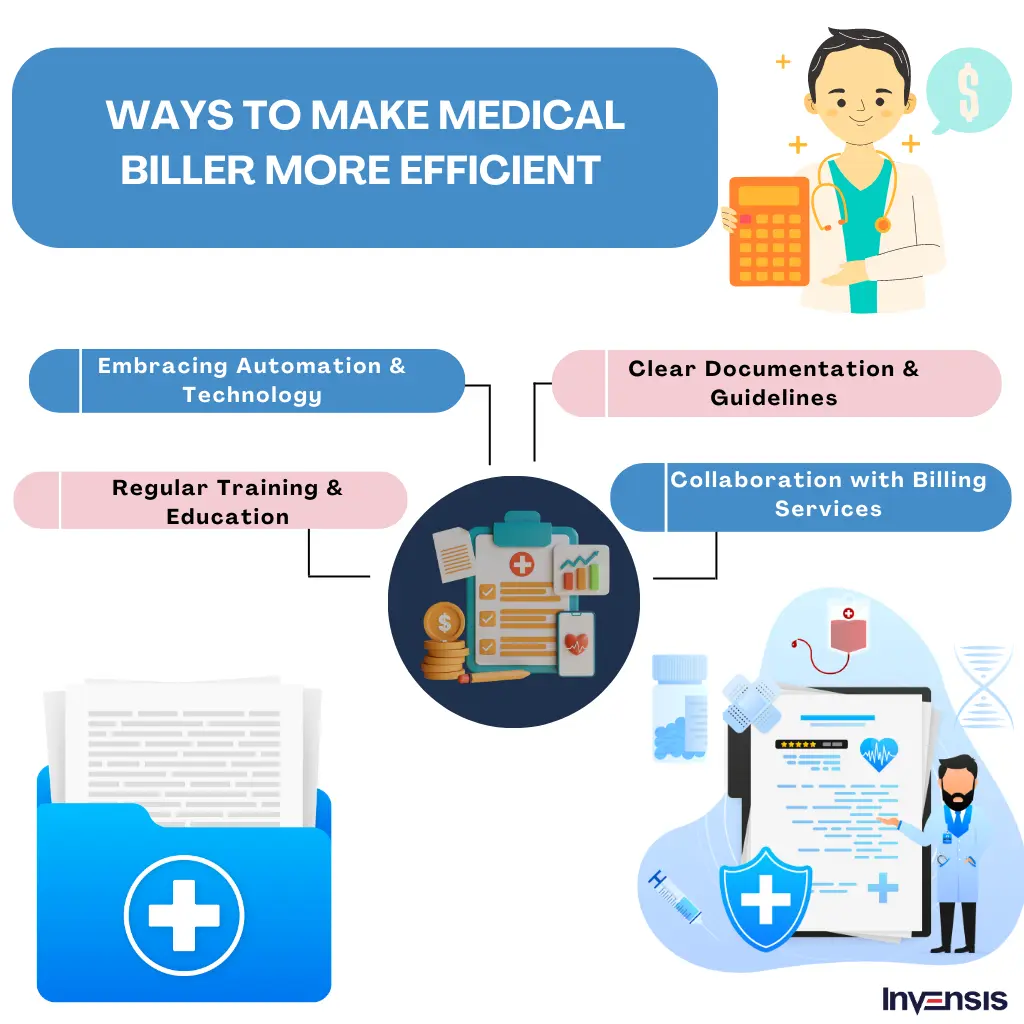
How To Improve Productivity of Medical Billers
Several factors can slow down the work of medical billers. Complex and constantly changing coding and billing regulations, insufficient or inaccurate documentation and incorrect patient information make their task error-prone. Additionally, high volumes of claims, claim rejections, and the need for appeals can overwhelm billers, impacting their productivity. A few proven ways to improve their productivity include:
1. Embracing Technology and Automation
Implementing billing software and technology solutions significantly streamline the medical billing process. Automation tools, in particular, can generate and submit claims electronically, reducing the chances of human errors.
2. Providing Clear Documentation and Coding Guidelines
Providing billers with comprehensive and up-to-date documentation and coding guidelines ensures accurate coding and reduces errors.
3. Imparting Routine Training and Education
Continuous training and education programs for medical billers are essential for keeping them updated with changing regulations, coding guidelines to avoid medical billing and coding errors, and industry best practices.
4. Improving Communication Between Teams
Encouraging clear and consistent communication between medical billers, healthcare providers, and other staff ensures that billers have access to accurate and timely information. Regular meetings and the use of communication platforms can help resolve queries quickly and reduce delays.
5. Conducting Regular Audits and Feedback Sessions
Routine audits of billing processes can identify recurring issues and areas for improvement. Providing constructive feedback to billers based on these audits helps refine their work processes and reduce errors.
6. Utilizing Data Analytics
Leveraging analytics tools to track billing trends, denial patterns, and performance metrics enables organizations to make data-driven decisions. These insights can help address inefficiencies and optimize the billing workflow.
7. Creating a Collaborative Work Environment
Fostering a supportive workplace culture where billers feel valued and encouraged to share challenges can improve morale and efficiency. Regular recognition of their contributions can boost motivation.
8. Streamlining Claim Denial Management
Developing a structured approach to manage claim denials, including predefined workflows for resubmissions and appeals, minimizes the time and effort spent on denied claims. Having a dedicated team or individual to handle this can also be effective.
9. Enhancing Patient Pre-Verification Processes
Ensuring accurate and complete patient information at the outset through robust pre-verification processes reduces billing errors and minimizes rework due to incorrect or missing details.
10. Partnering with Third-Party Billing Service Agencies
In some cases, delegating a part of the billing services to specialized companies can alleviate the workload of in-house billers. These include manual and time-consuming billing tasks.
Conclusion
The growing demand for healthcare services has increased the workload for medical billers, creating a need for more professionals in the field. Additionally, the complexity of medical billing regulations and coding systems requires specialized training and knowledge, making it challenging to find qualified individuals. Moreover, the rapid advancements in healthcare technology and electronic health records have resulted in a skill gap, as billers need to adapt to new software and processes.
Invensis has over 22 years of experience in assisting medical billers to simplify their tasks. We have a team of certified medical support professionals with adequate exposure to managing the diverse needs of medical billers. Partner with Invensis today to simplify and optimize your medical billing services and make the going easy for your billing team.
Frequently Asked Questions
Discover Our Full Range of Services
Click HereExplore the Industries We Serve
Click HereBlog Category
Related Articles

Optimize your store in 2026 with the best WooCommerce order management plugins. Automate order tracking, inventory, and customer service for success.
January 21, 2026
|

Find the leading accounting firms in Singapore trusted by businesses for audit, tax, and advisory services.
November 6, 2025
|

Explore the leading accounting firms in South Africa providing expert audit, tax, cloud accounting, and payroll services. Learn about their key features and unique offerings.
January 19, 2026
|
Services We Provide
Industries We Serve





.webp)