
 Revenue Cycle Management
Revenue Cycle ManagementThe Unbeatable Benefits of Electronic Claims Submission

Content
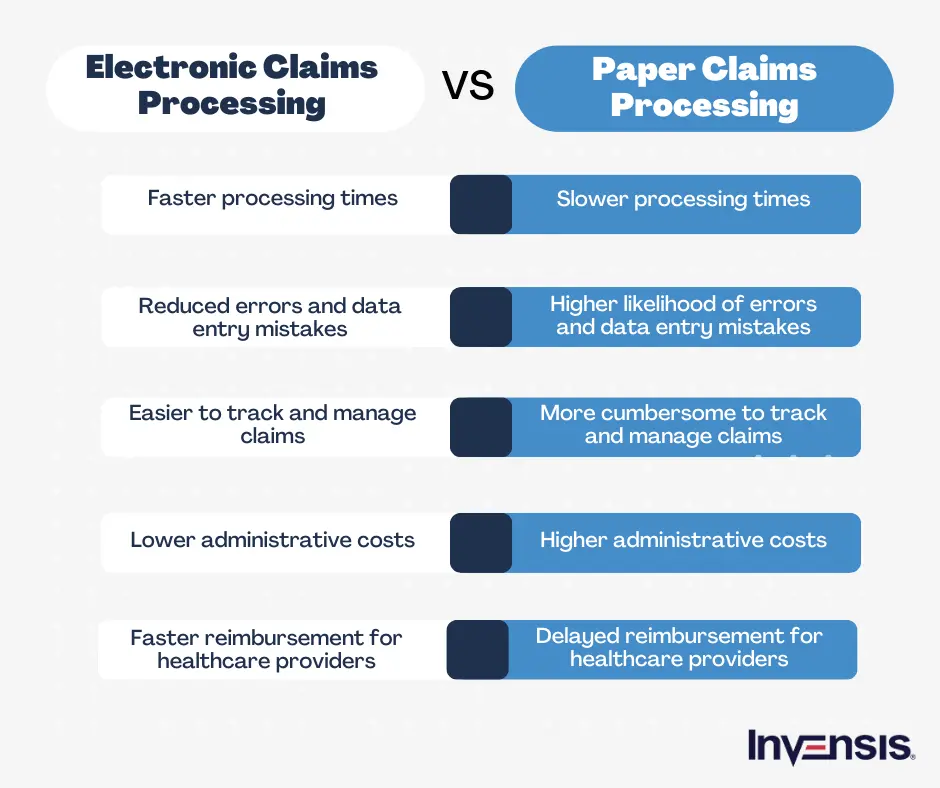
Electronic claims submission is a streamlined process that allows healthcare providers to submit medical claims electronically to insurance companies for reimbursement. This efficient method eliminates the need for paper-based claims, reducing errors and accelerating payment processing.
This technology has become a game-changer for healthcare organizations, insurers, and patients by replacing cumbersome paper-based systems with efficient electronic methods. By harnessing the power of electronic data interchange (EDI) systems, medical claims can now be transmitted seamlessly, securely, and accurately between healthcare providers and insurance companies, ensuring a smoother experience for all parties involved.
This blog will discuss the remarkable benefits of electronic claims submission to healthcare providers, insurance companies, and, most importantly, the patients they serve.
Understanding Electronic Claims Submission
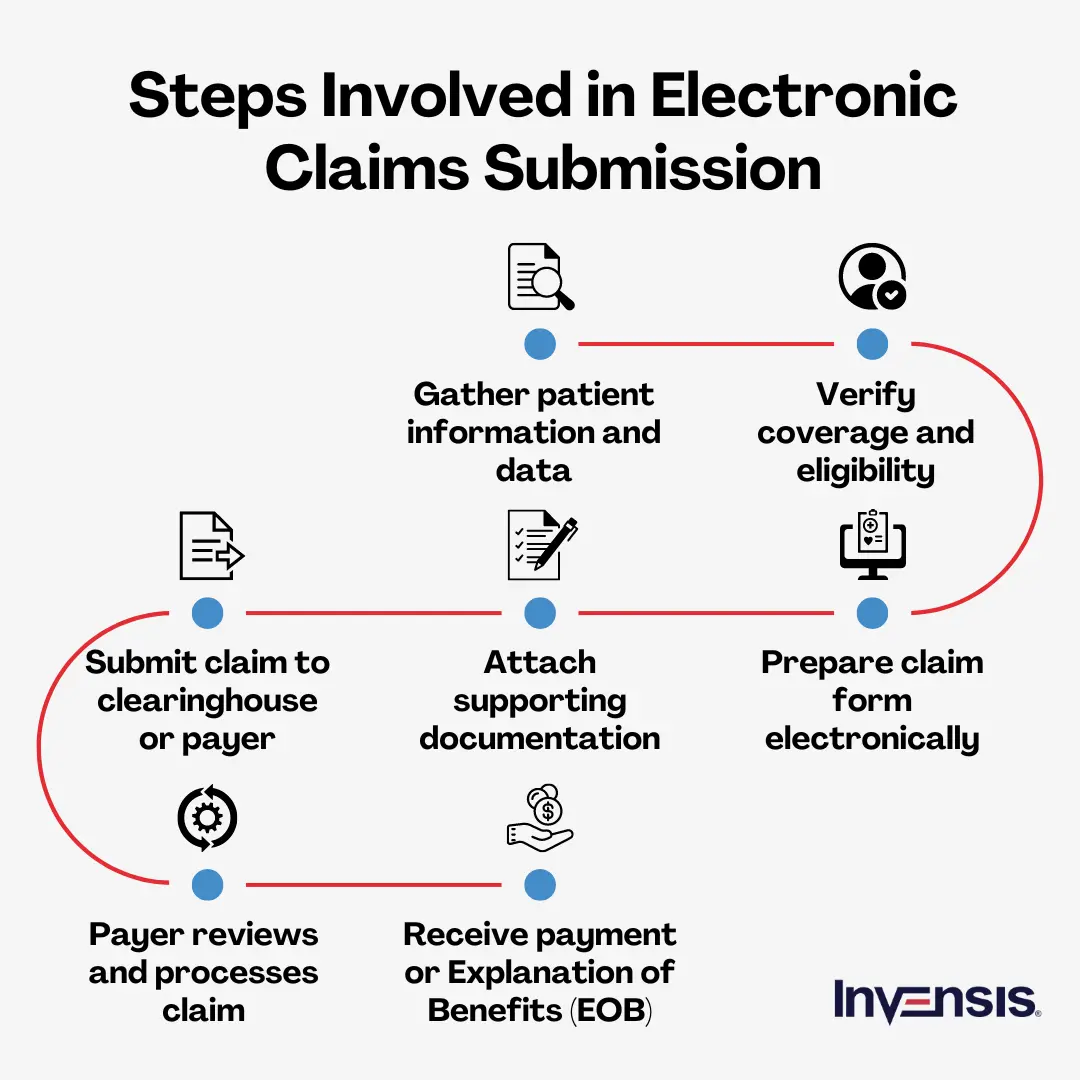
To understand the concept clearly, let's consider a medical practice that treats a patient covered by an insurance plan. Instead of manually filling out lengthy paper forms, the practice utilizes electronic claims submission. They enter patient information, diagnosis codes, and treatment details into their practice management software, which generates a standardized electronic claim.
Once reviewed for accuracy, the claim is electronically transmitted to the insurance company through a secure network. The insurer receives the claim, assesses its validity, and processes reimbursement accordingly. This digital workflow ensures faster turnaround times, minimizes claim denials, and enhances overall efficiency for healthcare providers, insurers, and patients.
Benefits of Electronic Claims Submission
Here are the top 7 electronic claims submission benefits:
1. Faster Claim Processing
- Automation and Efficiency: Eliminates manual processing and paperwork, enabling faster transmission and automated processing.
- Real-time Validation: Validate claims in real-time, reducing errors and minimizing the back-and-forth between providers and payers.
- Reduced Data Entry Errors: Pre-populated fields and data validation checks in electronic claims submission minimize errors, accelerating processing time.
- Streamlined Communication: Facilitate instant and secure transmission of claims information, improving communication between providers and payers for faster updates and payment details.
2. Reduced Errors
- Minimized Human Error: Reduce reliance on manual data entry, decreasing the likelihood of human errors, such as typos or miscalculations.
- Data Validation Checks: Identify errors or missing information upfront, allowing for timely corrections and reducing the need for resubmission.
- Standardization: Follow standardized formats and coding systems, reducing the chances of errors caused by misinterpretation or inconsistent data.
- Clear Documentation: Avoid missing or incomplete data, streamline the processing timeline, and minimize errors, which altogether improves clarity in documentation
- Enhanced Error Handling: Flag and highlight errors or inconsistencies in real-time, allowing providers to address them promptly.
3. Cost Savings
- Reduce Paperwork and Postage Costs: Minimize expenses by eliminating paper-based documentation and reducing postage costs through electronic claims submission.
- Minimize Errors and Rejections: Reduce the occurrence of errors and claim rejections to save resources and associated costs.
- Enhance Accuracy and Compliance: Ensure compliance with coding standards to avoid penalties and achieve cost savings.
- Improve Tracking and Reporting: Enhance tracking and reporting capabilities to analyze data and identify cost-saving opportunities.
4. Increased Accuracy
- Enhance Data Integrity: Improve accuracy and reliability of claim information by reducing manual data entry errors through electronic claims submission.
- Standardize Coding: Ensure claim coding and billing accuracy by enforcing standardized coding practices through electronic systems.
- Automate Validation: Validate claims automatically to identify and correct errors or inconsistencies, ensuring accurate and complete claim submissions.
- Enable Real-time Claim Edits: Allow immediate correction of errors or missing information in claims, enhancing accuracy and reducing the need for follow-up communication.
5. Improved Cash Flow
- Accelerate Payment Processing: Expedite reimbursement by processing electronic claims faster, improving cash flow for healthcare providers.
- Reduce Payment Delays: Minimize delays in payment by streamlining the claim adjudication process through electronic claims submission, ensuring a steady cash flow.
- Provide Prompt Claim Status Updates: Deliver real-time claim status updates, enabling providers to track progress and take necessary actions for faster payment and improved cash flow.
- Minimize Claim Rejections: Reduce claim rejections by utilizing automated validation checks, preventing payment delays and enhancing cash flow.
6. Enhanced Transparency and Tracking
- Increase Visibility: Enhance transparency by providing clear visibility into the claim submission and processing lifecycle through electronic systems.
- Track Claim Status: Enable real-time tracking of claim status, allowing providers to monitor the progress of their claims and stay informed throughout the process.
- Audit Trail: Maintain an electronic audit trail of claim submissions, edits, and updates, providing a transparent record of all interactions and ensuring accountability.
- Enhanced Data Analytics: Leverage data analytics capabilities to gain insights into claim performance, identify patterns, and optimize processes for improved transparency and tracking.
7. Streamlined Workflow and Productivity
- Automate Tasks: Streamline the workflow and boost productivity by automating manual tasks through electronic claims submission.
- Eliminate Paperwork: Enhance efficiency and productivity by eliminating paper-based documentation and manual handling.
- Expedite Data Entry: Accelerate productivity by expediting data entry through pre-populated fields, drop-down menus, and data validation checks.
- Centralize Data Access: Improve workflow efficiency by providing centralized access to claim-related data, eliminating the need for manual searching and enhancing productivity.
Conclusion
Electronic claims submission has become increasingly complex and challenging with the increased adoption of technology and the surge in claims volumes. The ever-changing landscape of healthcare policies, coding systems, and compliance requirements demands meticulous attention to detail and continuous adaptation. This complexity can overwhelm healthcare organizations, diverting their focus from patient care and burdening them with administrative tasks.
Delegating claims submission to a specialized service provider can alleviate these challenges and ensure a seamless claims process. Invensis possesses the expertise and experience to navigate electronic claims submission, staying up-to-date with the latest industry changes and regulations. Our medical claims processing services will handle all aspects of electronic claims submission, allowing you to focus on providing quality services to your patients. Contact us now to streamline your claims process and maximize your revenue potential.
Discover Our Full Range of Services
Click HereExplore the Industries We Serve
Click HereBlog Category
Related Articles

Optimize your store in 2026 with the best WooCommerce order management plugins. Automate order tracking, inventory, and customer service for success.
January 21, 2026
|

Find the leading accounting firms in Singapore trusted by businesses for audit, tax, and advisory services.
November 6, 2025
|

Explore the leading accounting firms in South Africa providing expert audit, tax, cloud accounting, and payroll services. Learn about their key features and unique offerings.
February 2, 2026
|
Services We Provide
Industries We Serve





.webp)