
 Revenue Cycle Management
Revenue Cycle ManagementThe Must-haves for Your Medical Billing Audit Checklist for 2026

Content
A medical billing audit systematically reviews and evaluates a healthcare provider's billing practices and financial documentation. It involves assessing the accuracy, completeness, and compliance of billing records, coding practices, and reimbursement processes. The primary goal of a hospital bill audit is to ensure that the billing practices align with industry standards, regulatory requirements, and insurance policies.
Medical billing audits help to identify and rectify potential errors, discrepancies, and fraudulent activities in billing processes. By conducting regular audits, healthcare providers can maintain compliance, minimize the risk of audits from insurance companies or government agencies, and prevent financial losses due to claim denials or legal penalties.
Audits also play a vital role in improving revenue cycle management. They help identify areas of improvement, such as coding accuracy, documentation quality, and billing efficiency. Healthcare providers can optimize reimbursement, reduce claim rejections, and enhance overall revenue generation by addressing these areas.
What is the Medical Billing Audit Checklist?
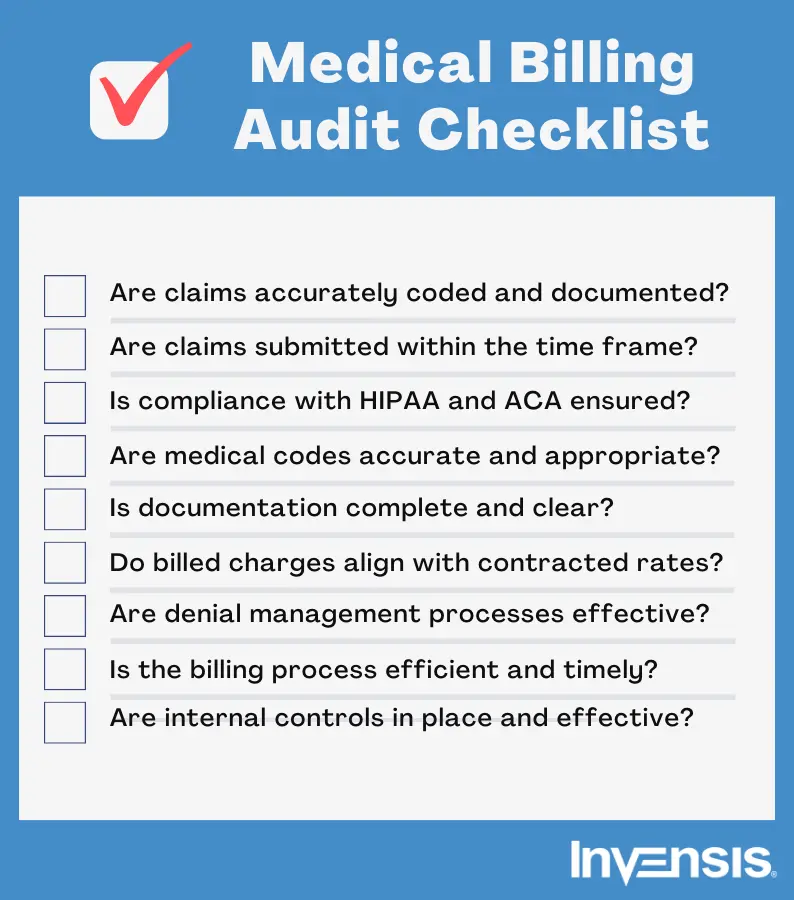
A medical billing audit checklist is a structured tool used to evaluate the accuracy, compliance, and efficiency of a healthcare provider’s billing processes. It ensures that medical claims are correctly coded, documented, and submitted in accordance with regulatory guidelines, such as HIPAA and CMS regulations.
The checklist typically includes verifying patient information, assessing coding accuracy, reviewing documentation completeness, checking for duplicate billing, and ensuring compliance with payer policies. By systematically identifying errors and inefficiencies, the checklist helps minimize claim denials, prevent fraud, and optimize revenue cycle performance. Regular use of a clinical billing audit checklist enhances financial stability, reduces legal risks, and improves overall operational efficiency for healthcare providers.
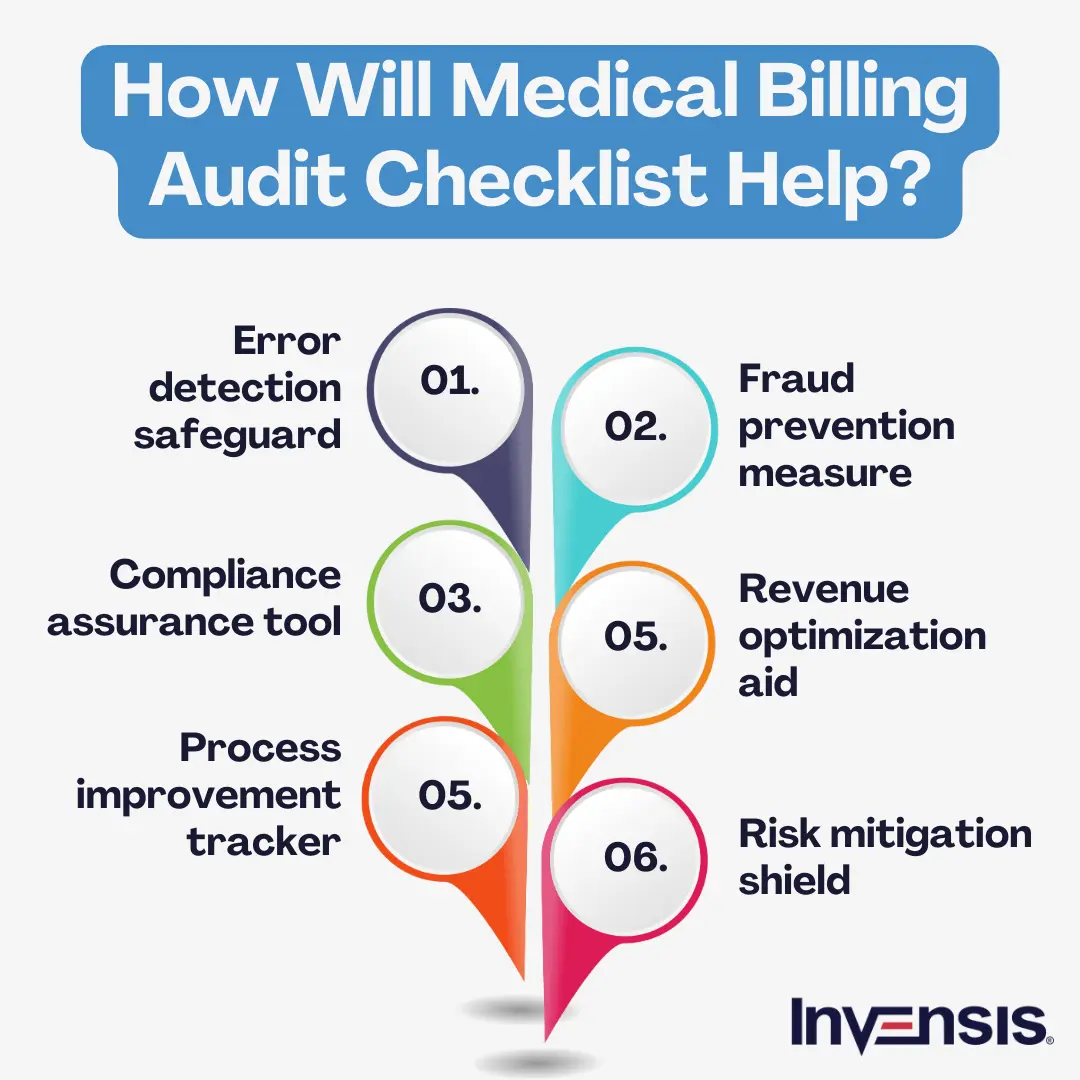
Benefits of Medical Billing Audit Checklist
Here are the key benefits of a well-structured audit checklist
- Error Reduction – Identifies and corrects coding, billing, and documentation errors, reducing claim denials.
- Compliance Assurance – Ensures adherence to HIPAA, CMS, and payer-specific regulations, minimizing legal risks.
- Revenue Optimization – Detects missed charges and incorrect claims, helping maximize reimbursements.
- Operational Efficiency – Streamlines billing workflows, reducing rework and improving processing speed.
- Fraud Prevention – Identifies duplicate billing and unauthorized claims, protecting against financial penalties.
- Improved Claim Approval Rates – Enhances accuracy in claim submissions, leading to faster reimbursements.
- Data-Driven Decision-Making – Provides insights into recurring issues, helping refine billing strategies.
- Stronger Patient Trust – Reduces billing errors and overcharges, improving patient satisfaction and transparency.
The Key Components of a Medical Billing Audit Checklist
Some of the key features of a comprehensive medical billing audit checklist should include the following key elements:
1. Claims Accuracy:
Accurate claims coding and documentation are essential for preventing denials, delays, and compliance risks. Ensuring that claims are submitted correctly and on time helps providers receive proper reimbursements while reducing potential billing errors.
2. Compliance with Regulations:
Compliance with industry regulations, such as HIPAA and the Affordable Care Act (ACA), is crucial for protecting patient data and ensuring ethical billing practices. Following these guidelines minimizes the risk of legal complications and financial penalties.
3. Coding Practices:
The correct use of ICD, CPT, and HCPCS codes is fundamental to accurate billing. Proper coding helps prevent issues such as undercoding, upcoding, and unbundling, ensuring that reimbursements align with services rendered.
4. Documentation Quality:
Comprehensive and clear medical records provide essential support for billed services. Well-maintained documentation ensures that medical necessity is established, claims are justified, and audits or reviews proceed smoothly.
5. Reimbursement Accuracy:
Aligning billed charges with payer contracts helps prevent revenue discrepancies. Consistently verifying reimbursement accuracy reduces financial losses from underpayments and prevents risks associated with overbilling.
6. Denial Management:
Understanding the root causes of claim denials and tracking patterns helps improve billing efficiency. A structured denial management process minimizes revenue loss and enhances claim approval rates.
7. Billing and Collections Process:
A streamlined billing and collections process contributes to timely payments and steady cash flow. Ensuring that claims are submitted on time and that patient invoices are clear helps reduce outstanding balances and improve revenue cycle performance.
8. Internal Controls:
Robust internal controls, including role-based access, audit trails, and security measures, help prevent fraud and financial discrepancies. Implementing effective safeguards ensures data integrity and compliance with financial regulations.
How to Implement an Audit Checklist
The best way to implement an audit checklist is by building a robust team of medical billing auditors and claims audit process.
The implementation involves several key steps:
- Establish the objectives and scope of the claims audit and determine what will be audited.
- Assemble a team with diverse expertise in coding, billing, compliance, and audit techniques.
- Create comprehensive audit procedures and checklists that outline the steps to be followed during the audit.
- Ensure the audit team receives proper training on billing regulations, coding guidelines, audit methodologies, and effective communication.
- Leverage technology solutions like billing software, data analytics tools, and automation features.
- Establish quality parameters for medical billing to maintain consistency and accuracy.
- Encourage open communication among team members and relevant stakeholders.
- Regularly assess the effectiveness of the medical billing audit process by monitoring key metrics and evaluating performance.
Conclusion
Implementing an in-house medical billing audit checklist poses challenges due to several factors. These include the complexity of medical billing regulations, frequent updates, resource-intensive training, software requirements, the need for specialized expertise, time constraints, potential biases, and the risk of overlooking critical areas. Delegating this task to specialized professionals may provide a more efficient and reliable solution.
A third-party partner specializing in medical billing can greatly assist in implementing an effective medical billing audit checklist. Their expertise and experience ensure comprehensive claims accuracy, compliance with regulations, and efficient reimbursement processes. At Invensis, we have been delivering medical billing services to healthcare businesses worldwide for the past two decades. Contact us for reliable and efficient medical billing solutions tailored to your needs.
Discover Our Full Range of Services
Click HereExplore the Industries We Serve
Click HereBlog Category
Related Articles

Optimize your store in 2026 with the best WooCommerce order management plugins. Automate order tracking, inventory, and customer service for success.
January 21, 2026
|

Find the leading accounting firms in Singapore trusted by businesses for audit, tax, and advisory services.
November 6, 2025
|

Explore the leading accounting firms in South Africa providing expert audit, tax, cloud accounting, and payroll services. Learn about their key features and unique offerings.
January 19, 2026
|
Services We Provide
Industries We Serve







.webp)